Healthcare workers in the operating room are exposed to radiation during a multitude of surgical procedures as visualisation may be required in orthopaedics, neurology, urology and cardiothoracic surgery.
New technologies and techniques have allowed clinicians to perform complex diagnostic and interventional procedures. Exposure to radiation in the operating room often occurs during the taking of standard x-rays and during fluoroscopy, often incorporating the use of a C-arm.
Medical radiography is a broad term used to describe the process of visualisation of the internal parts of the body using x-ray techniques. During a radiographic procedure, an x-ray beam is passed through the body. Fluoroscopy on the other hand is a type of medical imaging that shows a continuous X-ray image on a monitor, much like an X-ray ‘movie’ in essence. In order to perform these types of surgery the patient must be placed on a suitable operating table that allows for radiolucency.
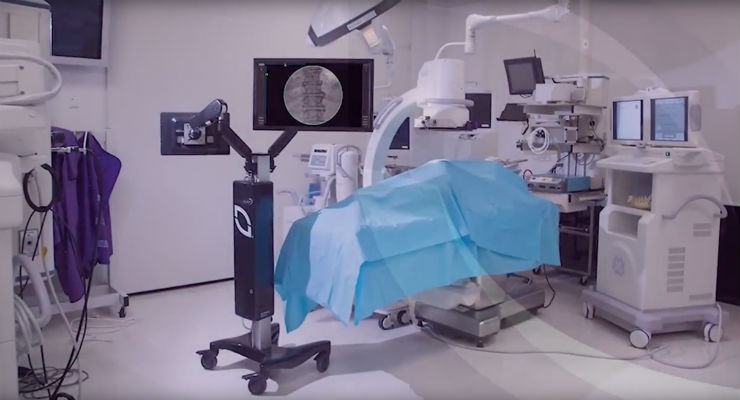
A hybrid operating room is a surgical theatre that is equipped with an appropriate theatre table and advanced medical imaging devices such as fixed C-Arms, CT scanners or MRI scanners. These imaging devices enable minimally-invasive surgery, which is less traumatic for the patient.
It has been estimated that in 1990 there were approximately 1.7 billion procedures performed involving the use of radiation and that increased to 4 billion in 2007. There has been more radiation deaths associated with medical uses than any other including Chernobyl. The risks of radiation exposure include developing a radiation induced cancer or cataracts, and disturbing the growth of a foetus in the case of a pregnant healthcare worker. During fluoroscopy there is a risk that the patient could sustain skin and underlying tissue injuries (burns).
It stands to reason that operating theatre personnel should embrace all possible techniques to protect themselves (and the patient) from over exposure to radiation.
How to protect yourself
- Always employ the ALARA principle (as low as reasonably achievable): simply put use the lowest radiation dose for the shortest time to achieve the required result
- Keep your distance: if possible stand 1.8m away from the radiation
- Keep the x-ray tube under the operating table: this reduces radiation scatter
- Wear protective clothing: this includes lead aprons, thyroid shield and lead glasses
- Always wear your dosimeter
- If you are wearing eye protection and thyroid protection, wear the dosimeter under your lead apron at waist height
- If you are not wearing eye protection and thyroid protection wear your dosimeter outside the apron at collar level
References:
- www.fda.gov/Radiation-EmittingProducts/…/MedicalImaging/…/ucm115354.htm
- http://www.fda.gov/Radiation-EmittingProducts/RadiationEmittingProductsandProcedures/MedicalImaging/MedicalX-Rays/ucm175028.htm
- https://web.stanford.edu/dept/EHS/prod/researchlab/radlaser/Hospital_Guidance_document.pdf
- Le Heron, J. Padovani, R. Smith, I. Czarwinski, R. 201. Radiation protection of medical staff. European Journal of Radiology, 76, 20-23.
- Source
OPERATING ROOM RADIATION
Radiation in the operating room is a prevalent issue in many situations – for the patient, surgeon, radiation technologist and operating room staff. Exposure to radiation has been associated with increased risk of cancer among surgeons in orthopedic hospitals (Mastrangelo, et al., 2005) , increased prevalence of breast cancer among female orthopedic surgeons (Chou, Chandran, & Harris, 2012), heightened risk of cardiovascular disease (Adams, Hardenbergh, Constine, & Lipshiltz, 2003), increased risk of melanoma among radiologic technicians (D. Michal Freedman , 2002), long term effects on the cataract (Hayes & Fisher, 1979), among many other detrimental and dangerous effects.
The effects of radiation are particularly relevant among spine surgeons, whose dose rate during fluoroscopically assisted pedicle screw insertion can be 10-12 times higher than a non-spinal thoracolumbar musculoskeletal procedure (Rampersaud, Foley, Shen, Williams, & Solomito, 2000). Here, we outline some techniques to reduce and mitigate radiation exposure and protect yourself and your patients in the operating room:
- Use Radiation Shielding
- Reduce Fluoroscopy Exposure
- Machine Vision Image-Guided Surgery
Use Radiation Shielding
Physical protection such as lead-lined shields, exiting the operating room, and surgeon/staff standing position are methods of shielding in order to reduce radiation exposure. The practice of wearing lead vests, aprons and thyroid collars is widely adopted as a primary method of shielding the surgeon and operating room staff from ionizing radiation. Proper practice of wearing and storing the aprons are crucial to the efficacy of wearing lead as a shield, however radiation blockage as low as 37.1% has been reported (Seung-Jae Hyun, 2016).
Reduce Fluoroscopy Exposure
Another way to reduce radiation in the operating room when using fluoroscopy is to follow the ALARA (as low as reasonably achievable) principles, designed to minimize radiation dose to the patient and surroundings. Using pulsed fluoroscopy rather than live or continuous fluoroscopy is one technique to reduce exposure. Using landmarks, manipulating the x-ray beam (collimation) and laser targeting are also ways to eliminate excess exposure (Kaplan, Liporace, & Yoon, 2016).
Along with these techniques, keeping hands out of the way of the x-ray beam, positioning the image intensifier close to the patient to reduce scatter, and increasing distance between yourself and the x-ray tube are methods of reducing your radiation dose during procedures (Kaplan, Liporace, & Yoon, 2016). Finally, establishing effective communication with the radiology technician is an essential part of eliminating unnecessary radiation if using fluoroscopy during procedures. However, the best way to reduce radiation and protect yourself in the operating room during navigated spinal procedures is by removing all radiation associated with navigation by performing machine-vision image-guided spine surgery.
Machine Vision Image-Guided Surgery (MvIGS)
In addition to improving surgical outcomes and screw accuracy, using a machine-vision image-guided surgery (MvIGS) system, such as the 7D Surgical System, eliminates all radiation associated with navigation from the operating room. Using only visible light to perform the registration in a totally sterile surgeon-controlled 20-second workflow, the patient’s anatomy is easily registered to a pre-operative scan.
The 7D Surgical System leverages machine-vision to segmentally register individual vertebrae in seconds, accounting for intersegmental motion and maintaining accuracy throughout the entire procedure as the spine is manipulated. Using machine-vision image guidance can also eliminate multiple intraoperative CT scans required when using radiation co-registration navigation systems.
This is particularly meaningful in pediatric scoliosis cases where multiple intraoperative scans are required for extended constructs due to the small imaging volume of intraoperative CT radiation co-registration systems. Instead, the 7D Surgical System utilizes the weight-based low dose preoperative CT, eliminating unnecessary additional spins and performing the CT in a controlled environment away from surgeons and OR staff.
There are numerous benefits to using machine-vision image-guided surgery systems such as the 7D Surgical System in your operating room, and it is the only way to eliminate all radiation associated with navigation in the OR while facilitating a fast, efficient and extremely accurate surgical experience.
References
- Adams, M., Hardenbergh, P., Constine, L., & Lipshiltz, S. (2003). Radiation-associated cardiovascular disease. Oncology Hematology, 55-75.
- Chou, L., Chandran, S., & Harris, A. (2012). Increased Breast Cancer Prevalence Among. Journal of Women’s Health, 683-9.
- D. Michal Freedman , A. S. (2002). Risk of melanoma among radiologic technologists in the United States. International Journal of Cancer.
- Hayes, B., & Fisher, R. (1979). Influence of a prolonged period of low-dosage x-rays on the optic and ultrastructural appearances of cataract of the human lens. British Journal of Ophthalmology, 457-64.
- Kaplan, D., Liporace, F., & Yoon, R. (2016). Intraoperative radiation safety in orthopaedics: a review of the ALARA (As low as reasonably achievable) principle. Patient Safety in Surgery, 10:27.
- Mastrangelo, G., Fedeli, U., Fadda, E., Giovanazzi, A., Scoizzato, L., & Saia, B. (2005). Increased cancer risk among surgeons in an orthopedic hospital. Occupational Medicine, 55:498-500.
- Rampersaud, Y., Foley, K., Shen, A., Williams, S., & Solomito, M. (2000). Radiation Exposure to the Spine Surgeon During Fluoroscopically Assisted Pedicle Screw Insertion. Spine, 2637-45.
- Seung-Jae Hyun, K.-J. K.-A.-J. (2016). Efficiency of lead aprons in blocking radiation − how protective are they? Heliyon.
- SOURCE