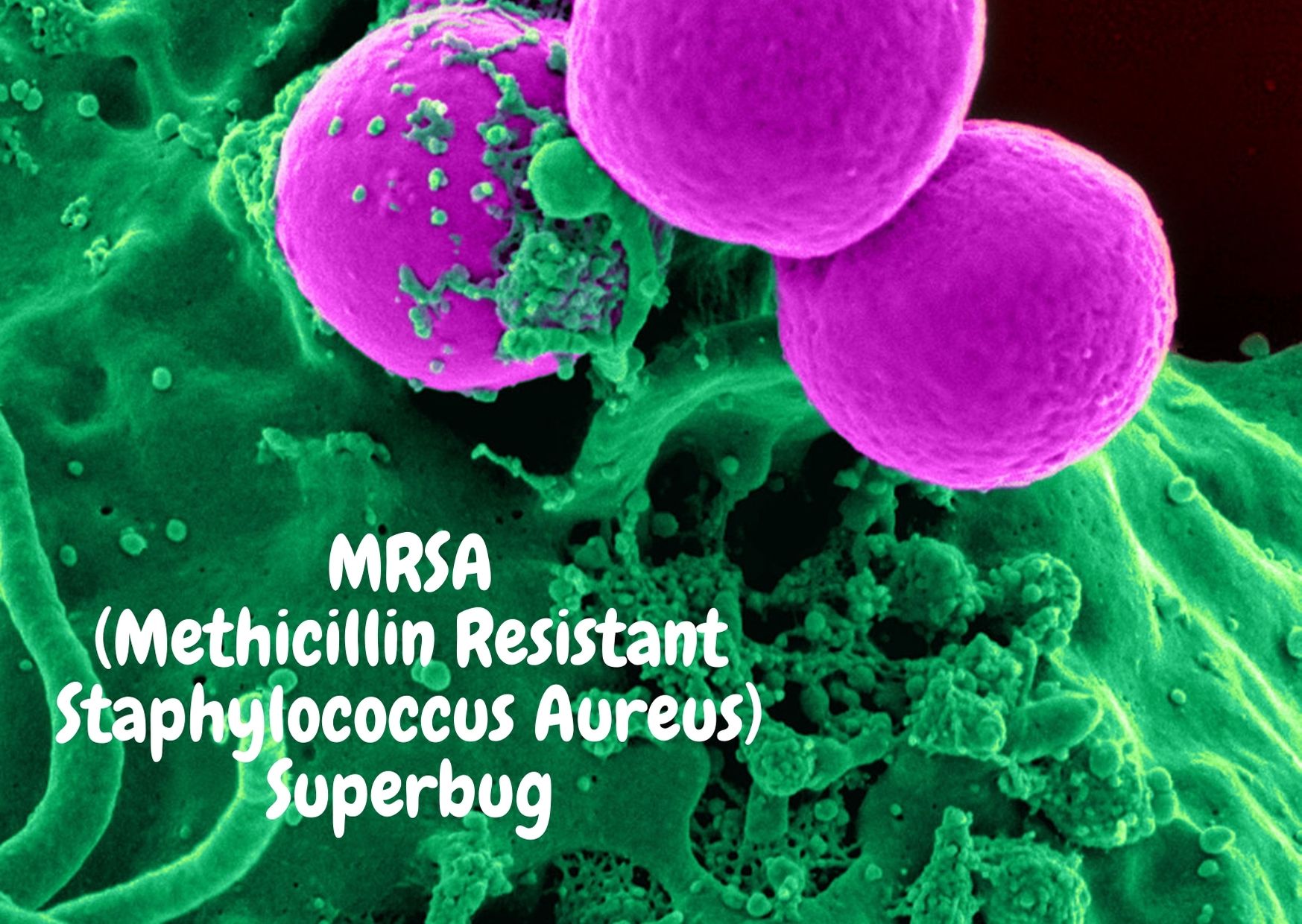
MRSA is the abbreviation for a specific type of bacteria (called “Staphylococcus aureus”) that is resistant to a class of antibiotics in the penicillin family including “methicillin.” The full name is Methicillin-resistant Staphylococcus aureus. Statistics reveal that about one in every three people carries staph aureus bacteria in their noses, and about one million people carry the MRSA type.
Over time, germs evolve to withstand treatment. Most staph is no longer treatable by the antibiotic penicillin. When penicillin was first used in the 1940’s, it could seemingly treat nearly any infection. As the use of penicillin increased over time (including some overuse and misuse) bacteria (including Staphylococcus aureus) became resistant.
As newer antibiotics were developed and used, bacteria became resistant to them as well, over time. Thus, there are a group of bacteria that are no longer sensitive to older antibiotics and a few bacteria that are resistant to nearly all of our current antibiotics.
MRSA is often referred to as a “super bug” because it is resistant to many antibiotics and can cause severe disease. It is especially common for people who spend a lot of time in hospital. There are, however, effective treatments for MRSA, and it is important to begin treatment as early as possible.
Staph infections occur only during close contact like sharing towels and razors, or rolling on the wrestling mat or football field with open wounds that are not protected with bandages. MRSA is preventable largely by common-sense hygiene using soap and water.
Diseases caused by MRSA are mostly skin infections, such as boils and abscesses.
Signs and Symptoms of MRSA
An MRSA infection usually begins when the resistant bacteria enter through the skin but MRSA can also invade the body in other areas such as the lungs. When entering through the skin, MRSA usually uses a small cut or a scratch for entry. In this case, early MRSA symptoms may include:
- A painful red bump or boil that may look similar to a “spider bite”
- A cluster of pimples
- A cut that begins to leak pus from it
If the infection progresses, the bump may become larger and more painful or be accompanied by spreading redness or tenderness. The bacteria can invade deeper into tissue and the blood stream causing fevers and chills, tiredness, cough or shortness of breath, rash, headache or worsening pain at infection site, and may cause more serious health problems and even death. People should seek medical attention as soon as they notice any symptom that is unusual so that the infection can be evaluated and treatment started early, if needed.
Symptoms of serious MRSA infection include:
- a high temperature
- aches and pains
- chills
- tiredness
- weakness
- confusion
If MRSA grow under skin, it can lead to a skin, fat or muscle infection.
Symptoms include:
- redness
- swelling
- warmth
- pain and sometimes pus from the skin.
Causes of MRSA infection
MRSA are more likely to cause an infection for people who are already very sick.
Healthy people are not usually at risk of MRSA infections. This includes children and pregnant women.
Things that put you at higher risk of MRSA infection
- Major surgery.
- Having a medical device inserted into your body, such as a catheter or IV line.
- Cancer treatment.
- Treatment in an intensive care unit or transplant ward.
How MRSA is spread
About 10% to 40% of healthy people have some form of the Staphylococcus aureus bacteria living on their body. This is part of the normal bacteria in our nose and, armpits, groin and other areas of skin. Skin-to-skin contact between people and contact between shared equipment can spread the bacteria. The bacteria can live on surfaces that come in contact with skin in common areas such as locker rooms, military barracks, and day care centers. The bacteria can also live on surfaces such as door handles, equipment, computer keyboards, and tabletops. Most people who come in contact with MRSA do not become infected and have no problem with it at all. It is only when the bacteria invade through the outer layer of skin or into our lungs that issues can arise.
Types of MRSA – HA-MRSA and CA-MRSA
A. Until the 1990s, MRSA was found mostly in hospitals and healthcare facilities, including nursing homes, dialysis units, and wound-care units. This type of MRSA is called healthcare associated MRSA (HA-MRSA). For the most part, HA-MRSA caused infections in people with weakened immune systems, older individuals, and also in people who had recently undergone surgery. In the 1990’s healthy people with no connection to hospitals or healthcare facilities also started getting MRSA infections. Some people at risk are athletes on sports teams, children in daycare, army recruits, and people in prisons. This type of MRSA is called community acquired MRSA (CA-MRSA).
Treatment of MRSA
If you carry MRSA, you may need treatment to remove it.
This usually involves washing with antibacterial shampoo and putting antibacterial cream in your nose.
Any skin irritation from treatment products should be mild. If you get a rash, stop treatment and ask your doctor or pharmacist for advice.
Preventing the spread of MRSA
During treatment, change your bedding, clothes and towel every day. Separate your laundry from others’ and wash at a high temperature.
Lower the risk of picking up and spreading MRSA in hospitals:
- clean your hands often
- use your own soap, flannel, sponge and razor
- Wash your hands often. Use an alcohol-based hand sanitizer when soap and water are not available
- Keep cuts and scrapes clean and bandaged until the skin heals
- Avoid touching other people’s scrapes and wounds or bandages without washing hands afterwards
- Do not share personal items, such as razors, towels, athletic equipment
- Shower with soap and water after all athletic events
- Clean high-touch surfaces regularly
If you are in hospital:
- limit contact with patients and keep away from their bed space
- avoid sharing food, newspapers or other personal items with patients
- tell staff if facilities in a hospital or clinic are not clean