The hip joint is a ball and socket joint between the top of the thigh bone and the pelvis which lies deep in the groin. Normally the surfaces of the ball and socket are covered by a smooth, low friction material called articular cartilage, which cushions the bones and lets them move easily. However, this can become worn and thin, a process known as osteoarthritis.
Hip function
The hip joint bears the full weight of your body. In fact, when you walk, the force transmitted through your hip can be up to three times your body weight.
As well as transmitting weight, the hip needs to be able to move freely to enable you to function normally. Muscles surrounding the hip such as your buttock (gluteal) and thigh muscles (quads) are also important in keeping your hip strong and preventing a limp.
The main reason for recommending a hip replacement is pain or loss of function due to arthritis.
A total hip replacement involves relining the hip socket (acetabulum) with a dense polyethylene or ceramic cup and replacing the ball at the end of the thigh bone (femur) with a stainless steel or ceramic ball on a stem that fits down the centre of the thigh bone. The aims of the hip replacement are to relieve the pain from your hip and to enable you to carry out your normal activities more comfortably.
Why do I need a Hip Replacement?
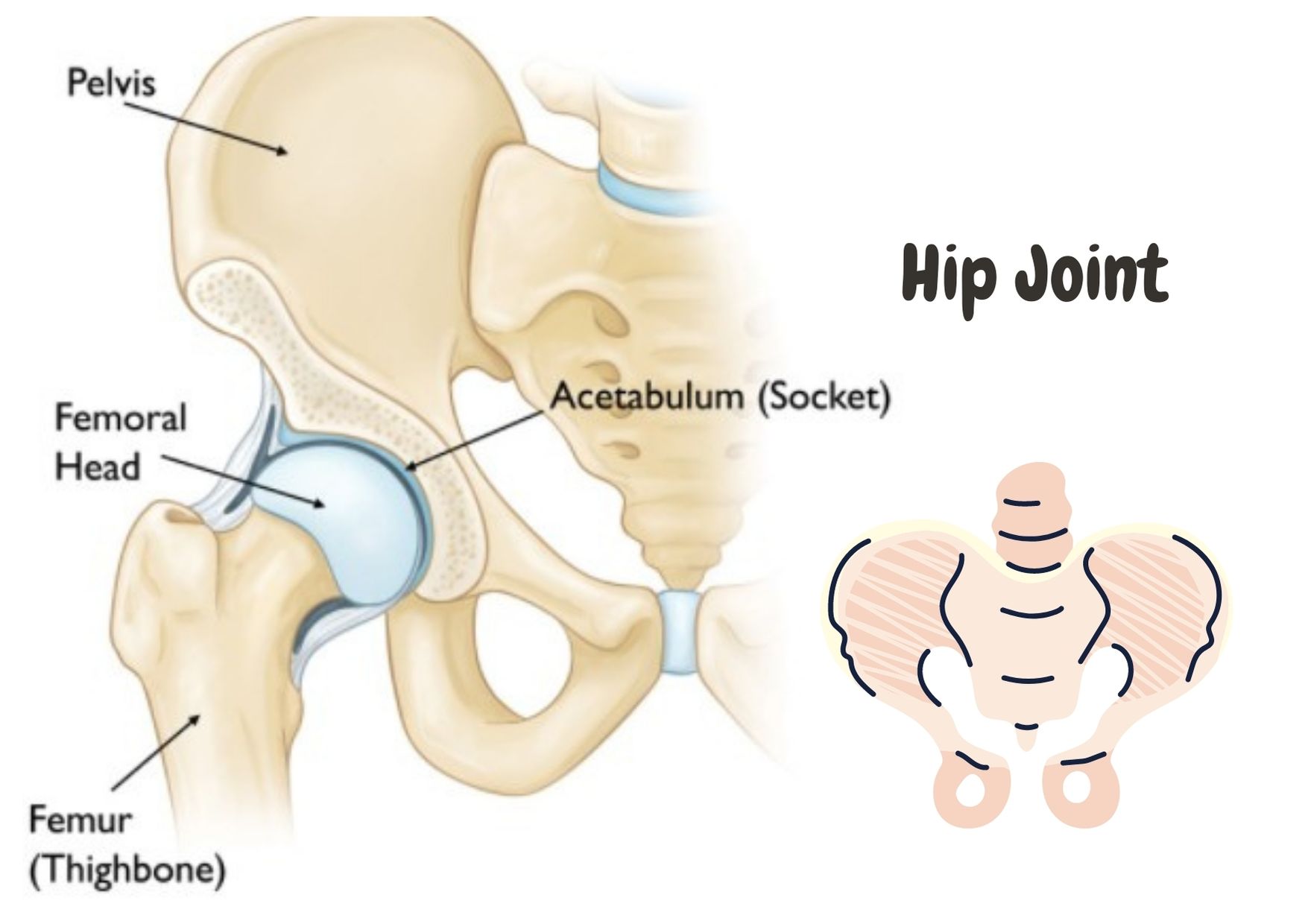
A ball (femoral head) at the top of your thigh bone (femur).
A socket (acetabulum) in your pelvis. Ligaments and muscles help keep the ball within the socket whilst allowing a large range of movement.
Revision Hip Surgery
Revision hip surgery is more complicated and more time consuming than first time hip replacements and the outcome is often less satisfactory. Complete pain relief is less common than in first time hip replacements and complication rates are higher. Infection rates are about double that in first time hips and dislocation rates are up to about five times higher. There is more risk to the nerves around the hip as they are often embedded in scar tissue and are therefore less easy to identify & protect during the operation. The mortality risk is also increased owing to the increased operating time and increased blood loss.
The type of revision hip operation required will depend on the method of failure of the first hip replacement:
Early infection (occurring within 3 months)
Signs of early infection:
- Ongoing drainage from the incision site
- Persisting wound redness
- Aching pain in the hip
- Fever
- A wound that bursts open, having been dry
Management:
The patient should reattend the hospital where the hip replacement was performed and tests will be done to confirm the infection. An operation to thoroughly wash out the joint will usually be offered, followed by a course, initially, of intravenous antibiotics and then oral antibiotics for up to three months. If the infection does not settle, then treatment is as for late infection.
Late infection
Signs of late infection:
- Onset of pain in a hip that was previously pain free
- Redness around the wound
- Presence of an abscess
- Fever and ill-health
Washout of the joint is seldom successful although it can be attempted if the x-ray appearances of the joint are perfect and if the onset of the infection appears to have been sudden.
Removal of the infected joint is almost always necessary. This is a difficult procedure, particularly where the hip replacement is well-fixed. Significant damage to host bone can occur whether removing a cemented or cementless implant. The operation should be done by an experienced hip surgeon.
Your surgeon will decide if it is possible to insert a new hip immediately or whether a temporary hip needs to be inserted while the infection is being treated. This will depend on a number of factors including the type of organism which caused the infection, the quality of host bone remaining and the type of new hip to be inserted (cemented or cementless).
If it is necessary to perform the revision operation in two stages, the definitive hip replacement will be inserted when the infection is eradicated. The timing between the two operations is usually a minimum of three months but may need to be significantly longer if the infection is slow to settle.
Recurrent dislocation
This is a very disappointing complication in an often otherwise well functioning hip. This can occur for a number of reasons:
- Lack of patient co-operation
- Slack soft tissues around the joint
- Soft tissue impingement due to scar tissue
- Malposition of components
This complication is difficult to treat and there is a risk that the hip will continue to dislocate despite revision surgery. The operation involves excision of scar tissue, repositioning of one or both components and application of a longer ball to tighten up the soft tissues. If a cemented hip is in position, the alignment of the components can be changed without removing all the well-fixed cement. The old components can be removed from within the cement and new components cemented into the old mantle in the appropriate position.
This revision technique makes the operation relatively straight forward. In very elderly patients with very slack tissues or with memory loss where post-operative instructions cannot be accurately followed, a locking socket may be required. This socket may also be required where there has been significant damage to the muscles around the hip, and in patients suffering from epilepsy, alcoholism, Parkinsonism or a stroke.
Aseptic loosening
One or both hip components may need to be changed and indeed may be necessary even if the component is not loose – the socket if it is worn and the stem if the ball is scratched and damaged. Loose components are easy to remove. The extent of bone loss is what can make reconstruction difficult. The surgeon will decide, based on his clinical experience and the degree of bone damage present, on the best form of reconstruction. The different methods include cemented or cementless components, with or without bone grafting, and the use of additional metalware such as screws, plates and cages to reinforce fixation.
Bone loss without loosening
This can be a totally asymptomatic process and reinforces the need for long-term review of hip replacements. It not uncommonly occurs behind cementless cups when the bearing surface is made of polyethylene but can also occur around the thigh bone component.
Although revision surgery can be fairly straight-forward when the socket is involved with bone grafting being performed behind the cup and a new bearing surface being introduced, re-operation can be a very major undertaking if the well-fixed components need to be removed. Significant bone damage can occur during the removal process requiring reconstruction with bone graft, supplemented by metal cages in the socket and bigger and longer stems in the thigh bone.