Most surgical fires involve electrosurgery and begin when the electrosurgical unit (ESU) is activated in oxygen-enriched environments. Severe burns and death are associated with these types of fires, which are often preventable. The Joint Commission on Accreditation of Healthcare Organizations (JCAHO) includes reduction of surgical fires among their 2005 Patient Safety Goals for ambulatory care and office-based surgery.1
PA-PSRS has received two reports of OR fires. In one case, a facial fire occurred involving the ESU active electrode in an oxygen-enriched environment. In the second case, inadvertent activation of the ESU ignited bone cement being used in an orthopedic procedure. Most OR fires occur during use of electrosurgery or electrocautery (i.e., hot wire) devices.
A number of other reports have been submitted by both hospitals and ambulatory surgical centers describing ESU-related electrical burns in the area of the face, neck, chest, and abdomen. While electrical burns, including “alternate site” burns, represent a fundamentally different mechanism of injury from surgical fires, both are known hazards of ESU use.
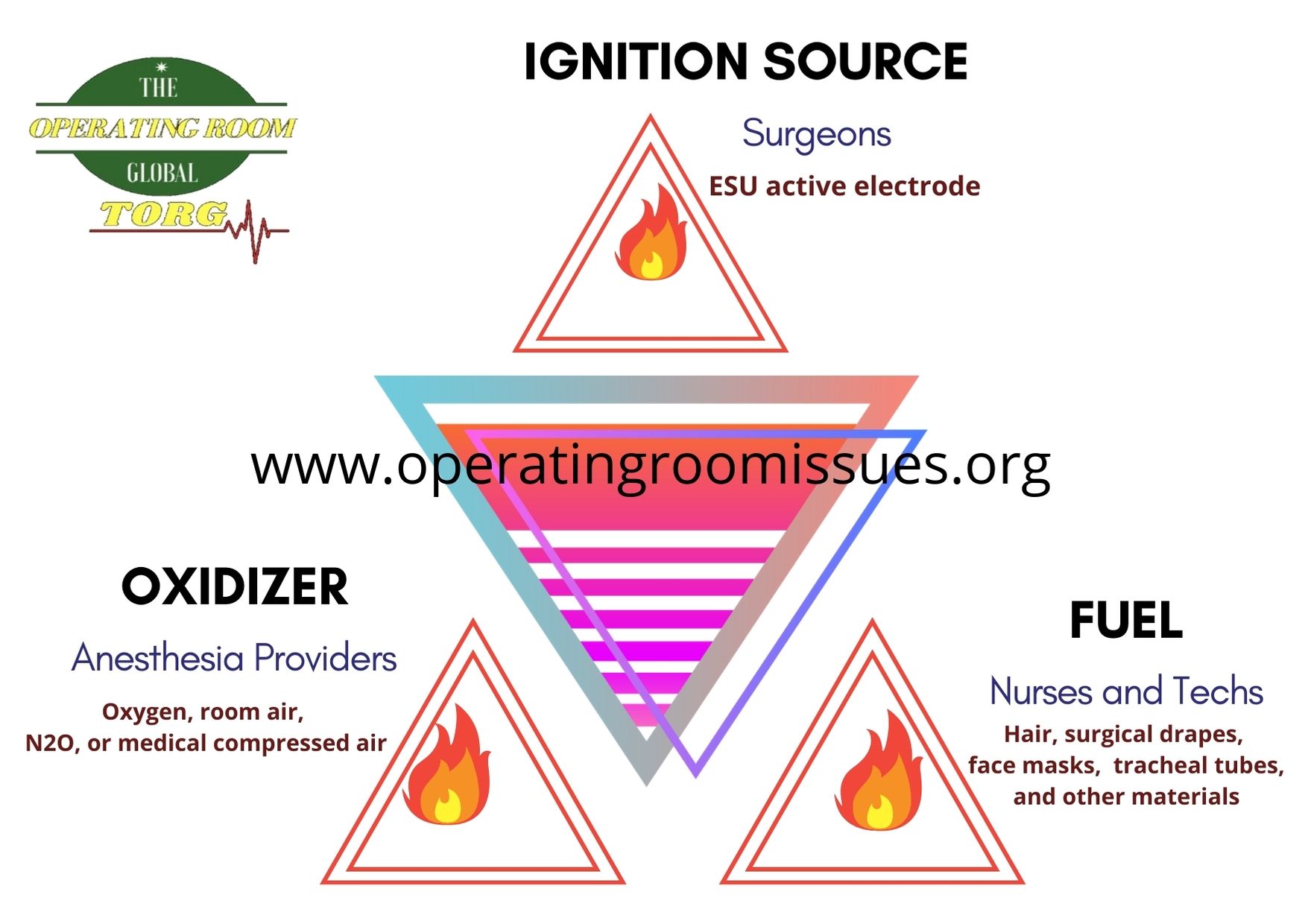
Fires require three elements
- An ignition source, such as an ESU active electrode.
- Oxidizers, such as oxygen, room air, N2O, or medical compressed air.
- Fuel, such as hair, surgical drapes, face masks, tracheal tubes, and other materials. Materials that don’t readily ignite and burn in room air (21% O2) will easily burn when the atmosphere is slightly enriched. For example, polyvinylchloride endotracheal tubes burn in 26% O2, and body hair will ignite in a flash fire and burn rapidly in oxygen-enriched atmospheres greater than approximately 50%.
Because oxygen is “heavier” than air, it collects in unexpected places, such as under surgical drapes in the head and neck area. It sometimes wells up through the drape fenestration into the surgical site. Fires in oxygen-enriched environments are easier to ignite, burn hotter and spread faster than fires do in normal air.
A further complication in the OR that increases the likelihood of a fire is that different people may be managing different aspects of the elements that must come together to cause a fire. For example, surgeons may handle the ignition source, anesthesiologists may deliver the oxidizers, and nurses may handle the fuels such as OR materials and flammable skin prepping agents. Communication among OR team members about specific fire risks is vital to reducing the risk of fire.
Manufacturers have tried to make equipment and surgical drapes safer but there simply is no clear engineering solution to the surgical fire problem. For example, there are two ways to activate the ESU, using the hand piece or the foot switch. Inadvertent activation has been reported with both methods in the clinical literature.
Clinicians address this problem by putting the ESU pencil in a holster when it is not in active use. Mayo stands are used for laparoscopic active electrodes, as they are too big for holsters. These preventive measures rely on trained staff to keep the patient and clinical personnel safe. If the ESU is inadvertently activated, it will often cause a burn and may cause a very serious fire. Both of those unfortunate circumstances are often preventable when a holster is consistently used.
In regard to drapes, it is a common misconception that fire-retardant drapes are available. They are not. This is primarily because the technology for making a fabric that will be fire-retardant in very high oxygen concentrations does not yet exist.
Practices that may help to reduce the risk of surgical fires include:
- Educating all members of the surgical team regarding the surgical fire hazard.
- Controlling potential ignition sources.
- Managing fuels, such as flammable surgical skin prep solutions.
- Minimizing the potential for medical gases to collect under surgical drapes.
An electrosurgical fire can occur under a number of scenarios.
A heat source such as an ESU can easily ignite alcohol vapors from alcohol-based prep solutions resulting in a surgical fire and/or skin burn. A heat source used at the surgical site can ignite alcohol or alcohol-based prep solutions if the solution is allowed to wick into the patient’s hair and linens or pool on the patient’s skin. If the patient is draped before the solution is completely dry, alcohol vapors can be trapped under the surgical drapes and channeled to the surgical site.
Two practices that may reduce the risk of fire or burns are:
- Ensuring that the prep solution does not soak into hair or linens – sterile towels can be used to absorb drips and runs during application.
- Ensuring that the prep solution is completely dry prior to draping, which may take a few minutes depending on the amount and location of the solution.
Electrosurgery-Related Burns
One of the most common ways for patients and surgical staff to experience skin burns is from inadvertent activation of an ESU (i.e., activated when not in contact with target tissue). Approximately 56% of all ESU-related events reported to PA-PSRS can be attributed to inadvertent ESU activation. Approximately 14% of those events are the result of not placing the active electrode handpiece in a safety holster between intentional activations. The remaining 42% of reports did not provide enough information to determine the reasons for the inadvertent activations.
A common practice is to place the active electrode handpiece on a flat part of the patient’s body, such as the abdomen, between uses. Inadvertent activation can easily occur if a staff member leans over or on the patient and makes contact with handpiece’s activation switch. The results can include a burn to the patient or the staff member, or ignition of a drape or other flammable material.
One of the easiest and most effective ways to avoid inadvertent activation is to place the active electrode handpiece in a safety holster that is provided with each new handpiece. For instruments that are too long for a holster (e.g., laparoscopic electrodes), the instrument can be placed on a table such as a Mayo stand that is nearby but away from the patient.
Making contact between an active electrode and another conductive surgical instrument, whether intentionally or unintentionally, can create a burn. For example, PA-PSRS received a report in which a patient experienced a “discoloration” along the vaginal mucosa where a conductive portion of the vaginal speculum was in contact with the vaginal wall. The reporting facility believed that unintentional contact with the speculum during activation of the ESU caused the discoloration.
In some cases, intentional contact is made between an active electrode and a conductive instrument such as a hemostat (a technique called “buzzing the hemostat”) in an attempt to control bleeding. In such cases an alternate site burn may occur to the patient if the conductive instrument is also in contact with non-target tissue during ESU activation.
Surgical staff must be aware of other instruments in the vicinity of the active electrode to avoid or reduce the potential for burns. Contacting the active electrode with the conductive instrument prior to ESU activation reduces the likelihood of arcing, thereby reducing the likelihood of an alternate site burn.
PA-PSRS has received four reports involving patients wearing jewelry upon entering the OR. In one report the patient refused to remove two nipple rings prior to an appendectomy. In a second report, two finger rings were removed from the patient while in the OR. The third report described a patient who was unable to remove a wedding band, and in the fourth report the surgeon assured the patient that her belly ring could remain in place during a laparoscopic hysterectomy.
Most healthcare facilities have policies against patients wearing jewelry during surgical procedures, especially those involving electrosurgical instruments. Many institutions developed policies for fear of patients being burned on the part of the body where the conductive jewelry is located if electrosurgery is applied.
Jewelry need not be removed to avoid burns during electrosurgery. The risk of an alternate-site burn (i.e., those away from the return electrode site) from the electrical conductivity of jewelry is extremely low. Alternate-site burns are more closely associated with contact between the patient and a grounded conductive object – jewelry does not greatly contribute to that risk. Nevertheless, some healthcare facilities encourage patients to remove jewelry to avoid the possibility of loss or theft.
There is a different reason to remove jewelry or cover it with tape or gauze during electrosurgery: to help prevent any sharp edges of the jewelry from scratching the insulation layer of active electrodes or cables of the ESU. Damage to the insulation layer can lead to an unintentional burn from electric current passing from the damaged site to the patient or staff. Prior to deciding on leaving jewelry in place, consider any potential for swelling, especially finger rings during surgery or recovery.
The information in this article is not comprehensive with respect to electrosurgery-related fires or burns, but it accurately presents some of the most common problems associated with electrosurgery. Certainly, due diligence and a good understanding of the technical aspects of electrosurgery on the part of surgical staff will greatly reduce or eliminate the risk of electrosurgery-related injuries or fires from occurring.
When performing electrosurgery:
- Use extreme caution in oxygen-rich environments, particularly during head and neck surgery.
- Be mindful of flammable objects near the surgical site.
- Use coagulation techniques only when clinically necessary.
- Keep the ESU handpiece in the safety holster between activations.
The following resources may help you learn more about this important subject.
Print Resources
- De Richemond A and Bruley ME. Head and neck surgical fires. Chapter 37. In: Eisele DW, ed. Complications in head and neck surgery. St. Louis (MO): Mosby; 1992;492-508.
- ECRI. Fire safety poster [online]. Available from Internet: http://www.mdsr.ecri.org.
- ECRI. A clinician’s guide to surgical fires: How they occur, how to prevent them, how to put them out [guidance article]. Health Devices 2003;32(1):5-24. Summary available from Internet: http://www.guideline.gov/summary/summary.aspx?doc_id=3688&nbr=2914&string=fire.
- Flowers J. Code red in the OR—implementing an OR fire drill. AORN J 2004 Apr;79(4):797-805.
- Joint Commission on Accreditation of Healthcare Organizations. 2005 ambulatory care national patient safety goals [online]. Available from Internet: http://www.jcaho.org/accredited+organizations/patient+safety/05+npsg/05_npsg_amb.htm.
- Joint Commission on Accreditation of Healthcare Organizations. Preventing surgical fires [online]. Sentinel Event Alert 2003 Jun 24;29. Available from Internet: http://www.jcaho.org/about+us/news+letters/sentinel+event+alert/sea_29.htm.
- National Fire Protection Agency. NFPA 99: standard for health care facilities. 2002.
- National Fire Protection Agency. NFPA 115: recommended practice on laser fire protection. 1999.
- Valley Lab Hotline News. OR fires! Minimizing the risk [online]. Available from Internet: http://www.valleylab.com/displaynews.cfm?articlepageid=221&pageid=221&menu=education&old=124.
Supplemental Material
Educational Videos
- Association of periOperative Registered Nurses (AORN). Fire Safety in the Perioperative Setting . Denver (CO).
- Medfilms. Operating room fire . Tucson (AZ).
- Molnlycke Health Care. Fire safety in the OR: A triad of prevention . Goteborg (Sweden).
Notes
- Joint Commission on Accreditation of Healthcare Organizations. National patient safety goals for 2004 and 2005 [online]. [Cited 2004 Aug 11.] Available from Internet: http://www.jcaho.org/accredited+organizations/patient+safety/05+npsg/05_npsg_amb.htm.
- Pennsylvania Patient Safety Reporting System. Patient Safety Advisory. Electrosurgical units and the risk of surgical fires [online]. Available from the internet: http://www.psa.state.pa.us/psa/lib/psa/advisories/sept_2004_advisory_v1_n3.pdf.
- Pennsylvania Patient Safety Reporting System. Patient Safety Advisory. Risk of fire from alcohol-based solutions [online]. Available from Internet: http://www.psa.state.pa.us/psa/lib/psa/advisories/june_2005_advisory_v2_n2.pdf.
- ECRI. Ignition of debris on active electrodes [Hazard Report]. Health Devices 1998 Sep-Oct;(27):9-10:367-70.
- ECRI. Allowing patients to wear jewelry during surgical (and electrosurgical) procedures {Talk to the Specialist}. Health Devices 1997 Nov;26(11):441-2.